Oral Paper Presentation
Annual Scientific Meeting
Session: Presidential Plenary Session 2
8 - Randomized Controlled Trial Comparing the Efficacy and Cost of Two Novel Through the Scope Tissue Approximation Devices
Monday, October 23, 2023
9:42 AM - 9:54 AM PT
Location: Ballroom B
- SJ
Salmaan A. Jawaid, MD
Baylor College of Medicine
Houston, TX
Presenting Author(s)
Salmaan A. Jawaid, MD, Noor Zabad, , Ahmad Aboelezz, MD, Gehad Daba, MD, Fares Ayoub, MD, Michael Mercado, , Mai A. Khalaf, MD, Tara Keihanian, MD, Mohamed O. Othman, MD
Baylor College of Medicine, Houston, TX
Introduction: Closure techniques for large endoscopic resection defects (ERD) continue to evolve. Focus has shifted from one step tissue apposition to tissue approximation first, which allows healthy mucosal tissue to be brought in close proximity to each other, followed by complete closure. In this study we compare the clinical efficacy and cost of two novel through the scope (TTS) tissue approximation devices in the management of large ERD.
Methods: In a single-center RCT study conducted from Aug 2022 to May 2023, we compared the effectiveness of the dual-action tissue clip (DAT) and the TTS tack/suture device (TSD) for closure of ERD measuring >20mm (width) and >30mm (length). Closure method was randomly assigned. The primary outcome was tissue approximation and approximation cost. Tissue approximation was defined as having ≤15mm of visible resection bed, using only the assigned device. Complete closure, without any visible resection bed remaining, was achieved using standard TTS instruments. Both outcomes were verified by a trained third-party observer.
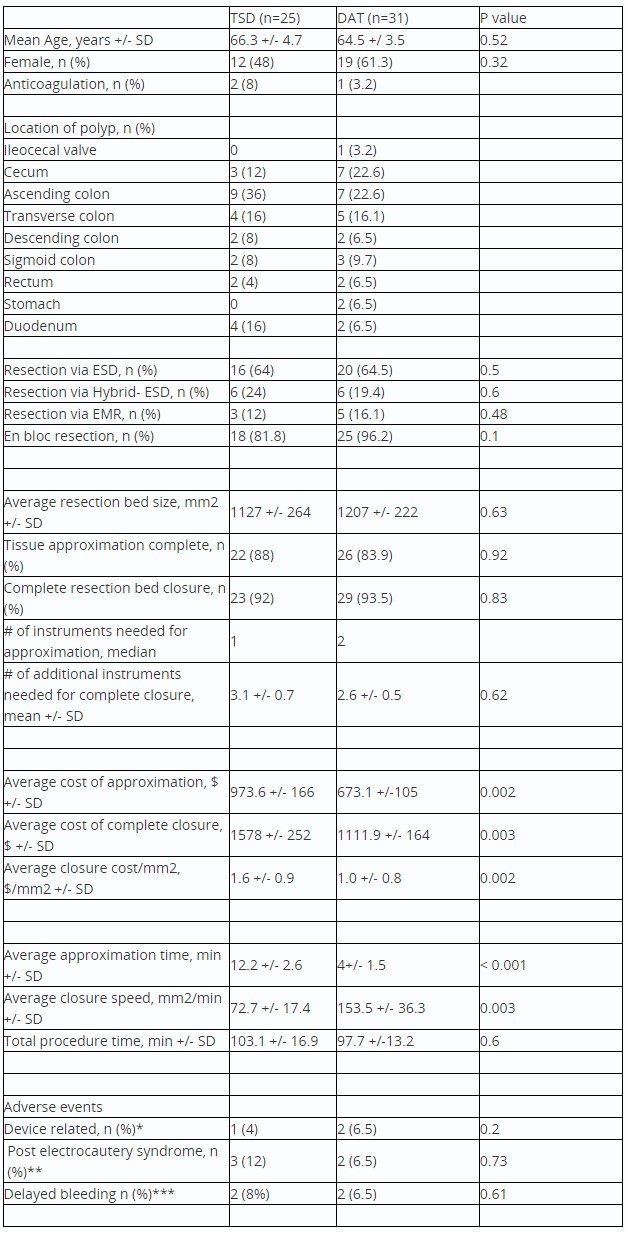
Results: 56 patients were included (Table 1). Tissue approximation (88% vs 83.9%, p =0.92) and complete closure rates (92% vs 93.5%, p=0.83) were similar for both TSD and DAT groups, respectively. 60% (n=3) of DAT failures (Fig 1) underwent successful tissue approximation using TSD. 33% (n=1) of TSD failures, underwent successful tissue approximation using the DAT clip. Multivariable analysis demonstrated a circular ERD shape was 21.1 times more likely to be associated with approximation failure (p=0.004) in both groups. TSD was able to approximate all 4 duodenal ERD, while DAT was unable to approximate any duodenal ERD. Approximation cost ($973.6 vs $673.1, p=0.002) and closure cost/mm2 ($1.6/mm2 vs $1.0/mm2, p=0.002) were lower in the DAT arm. Tissue approximation time (12.2 minutes vs 4 minutes, p< 0.0001) and closure clinical speed (72.7 mm2/min vs 153.5mm2/min, p= 0.003) was faster in the DAT group. Mild device related adverse events occurred once in the TSD group vs twice in the DAT group. Clinically significant delayed bleeding occurred once in both groups, while patients resumed anticoagulation.
Discussion: In this RCT, both TTS approximation devices equally facilitate approximation and closure of large ERD. Tissue approximation with the DAT clip was faster and more cost-effective than TSD for most resection bed shapes and sizes. However, TSD may be more effective for approximation of duodenal ERD.

Disclosures:
Salmaan A. Jawaid, MD, Noor Zabad, , Ahmad Aboelezz, MD, Gehad Daba, MD, Fares Ayoub, MD, Michael Mercado, , Mai A. Khalaf, MD, Tara Keihanian, MD, Mohamed O. Othman, MD, 8, Randomized Controlled Trial Comparing the Efficacy and Cost of Two Novel Through the Scope Tissue Approximation Devices, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Baylor College of Medicine, Houston, TX
Introduction: Closure techniques for large endoscopic resection defects (ERD) continue to evolve. Focus has shifted from one step tissue apposition to tissue approximation first, which allows healthy mucosal tissue to be brought in close proximity to each other, followed by complete closure. In this study we compare the clinical efficacy and cost of two novel through the scope (TTS) tissue approximation devices in the management of large ERD.
Methods: In a single-center RCT study conducted from Aug 2022 to May 2023, we compared the effectiveness of the dual-action tissue clip (DAT) and the TTS tack/suture device (TSD) for closure of ERD measuring >20mm (width) and >30mm (length). Closure method was randomly assigned. The primary outcome was tissue approximation and approximation cost. Tissue approximation was defined as having ≤15mm of visible resection bed, using only the assigned device. Complete closure, without any visible resection bed remaining, was achieved using standard TTS instruments. Both outcomes were verified by a trained third-party observer.
Results: 56 patients were included (Table 1). Tissue approximation (88% vs 83.9%, p =0.92) and complete closure rates (92% vs 93.5%, p=0.83) were similar for both TSD and DAT groups, respectively. 60% (n=3) of DAT failures (Fig 1) underwent successful tissue approximation using TSD. 33% (n=1) of TSD failures, underwent successful tissue approximation using the DAT clip. Multivariable analysis demonstrated a circular ERD shape was 21.1 times more likely to be associated with approximation failure (p=0.004) in both groups. TSD was able to approximate all 4 duodenal ERD, while DAT was unable to approximate any duodenal ERD. Approximation cost ($973.6 vs $673.1, p=0.002) and closure cost/mm2 ($1.6/mm2 vs $1.0/mm2, p=0.002) were lower in the DAT arm. Tissue approximation time (12.2 minutes vs 4 minutes, p< 0.0001) and closure clinical speed (72.7 mm2/min vs 153.5mm2/min, p= 0.003) was faster in the DAT group. Mild device related adverse events occurred once in the TSD group vs twice in the DAT group. Clinically significant delayed bleeding occurred once in both groups, while patients resumed anticoagulation.
Discussion: In this RCT, both TTS approximation devices equally facilitate approximation and closure of large ERD. Tissue approximation with the DAT clip was faster and more cost-effective than TSD for most resection bed shapes and sizes. However, TSD may be more effective for approximation of duodenal ERD.

Figure: Figure 1: Outcomes of device failures in DAT and TSD groups
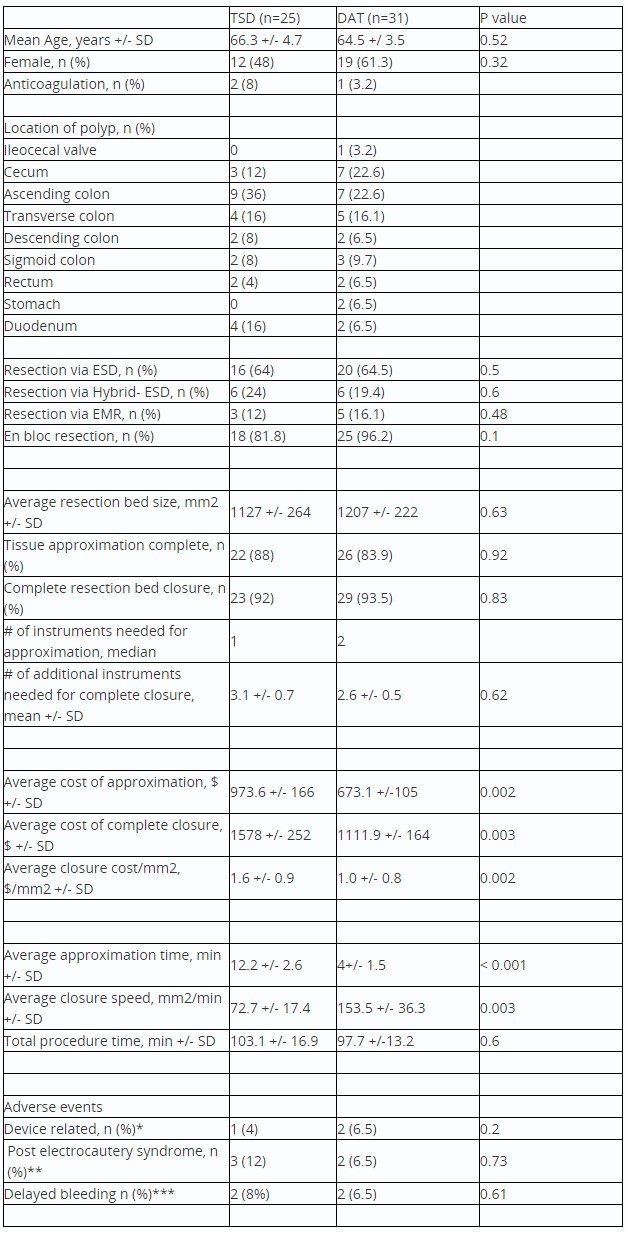
Table: Table 1: Clinical outcomes for subjects undergoing tissue approximation and defect closure after endoscopic resection
*All related to intraprocedural bleeding occurring from device trauma. All self-limited except one DAT patient who required coagulation grasper to treat
** All patients treated with antibiotics at home and did not require admission
*** One patient in both groups had self-limited bleeding, resolving without admission or intervention. One patient in X-tack group required PRBC, hospital admission and endoscopic treatment, X-tack was in place. One patient in the DAT group required intervention with evidence that the DAT clip had dislodged. Both patients were on anticoagulation.
*All related to intraprocedural bleeding occurring from device trauma. All self-limited except one DAT patient who required coagulation grasper to treat
** All patients treated with antibiotics at home and did not require admission
*** One patient in both groups had self-limited bleeding, resolving without admission or intervention. One patient in X-tack group required PRBC, hospital admission and endoscopic treatment, X-tack was in place. One patient in the DAT group required intervention with evidence that the DAT clip had dislodged. Both patients were on anticoagulation.
Disclosures:
Salmaan Jawaid: Boston Scientific – Consultant. ConMed – Consultant. CREO Speedboat – Consultant. DiLumen – Consultant.
Noor Zabad indicated no relevant financial relationships.
Ahmad Aboelezz indicated no relevant financial relationships.
Gehad Daba indicated no relevant financial relationships.
Fares Ayoub indicated no relevant financial relationships.
Michael Mercado indicated no relevant financial relationships.
Mai Khalaf indicated no relevant financial relationships.
Tara Keihanian: ConMed – Consultant. Lumendi – Consultant. Neptune Medical – Consultant.
Mohamed Othman: AbbVie Inc. – Consultant, Grant/Research Support. Apollo – Consultant. Boston Scientific Coporation – Consultant, Grant/Research Support. ConMed – Consultant, Grant/Research Support. Creo Medical – Consultant. Lucid Diagnostics – Grant/Research Support. Lumendi – Consultant. Olympus – Consultant.
Salmaan A. Jawaid, MD, Noor Zabad, , Ahmad Aboelezz, MD, Gehad Daba, MD, Fares Ayoub, MD, Michael Mercado, , Mai A. Khalaf, MD, Tara Keihanian, MD, Mohamed O. Othman, MD, 8, Randomized Controlled Trial Comparing the Efficacy and Cost of Two Novel Through the Scope Tissue Approximation Devices, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.


