Oral Paper Presentation
Annual Scientific Meeting
Session: Presidential Plenary Session 1
6 - Early Onset Colorectal Cancer Mortality Is Higher in the Southeast US and Significantly Associated With Poor Food Environment
Monday, October 23, 2023
8:50 AM - 9:00 AM PT
Location: Ballroom B
.jpg)
William K. Oelsner, MD
University of Tennessee HSC College of Medicine Chattanooga
Chattanooga, TN
Presenting Author(s)
Award: Outstanding Research Award in the Colon Category (Trainee)
William K. Oelsner, MD, Arslan Kahloon, MD, Priya Vijayvargiya, MD
University of Tennessee HSC College of Medicine Chattanooga, Chattanooga, TN
Introduction: Since the 1990s, there has been an alarming rise in the incidence and mortality of early onset colorectal cancer (EOCRC) in the US. While the exact mechanism of this rise is still unknown, there have been several proposed factors including obesity, diet, physical inactivity, and environmental exposures. The food environment (FE) is the physical, economic, and sociocultural context in which populations obtain and consume food. This is the first study to critically examine the relationship of food environments, dietary patterns, and food costs with respect to EOCRC mortality on a national level.
Methods: This national retrospective cohort study examined the county level mortality of EOCRC using data from the National Programs of Cancer Registries and Surveillance, Epidemiology and End Results Program. FE data was obtained from the Food Environment Atlas and Community Health Rankings Program. Individuals aged 20-49 residing in the contiguous US from 1999 to 2020 with colorectal cancer were included in the study. SEER*Stat was used to calculate county mortality rates; GraphPad was used to calculate Pearson correlation coefficients and unpaired t-tests with Welch correction; ArcGIS Pro was used for mapping and spatial analysis.
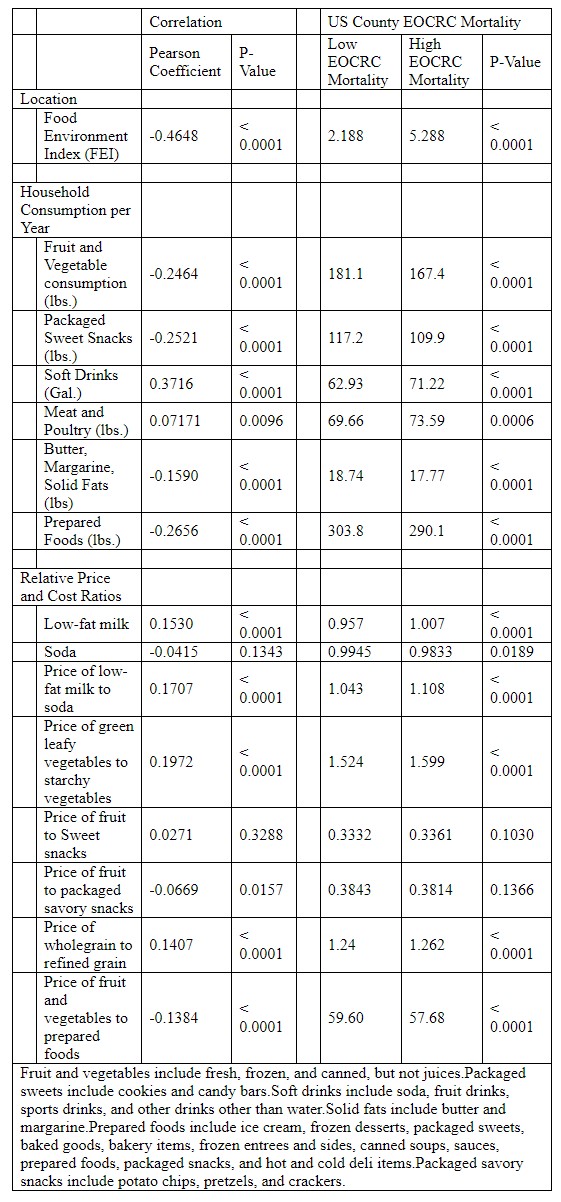
Results: 68,495 people from 1,307 counties met inclusion criteria. The greatest density of EOCRC mortality was concentrated in the Southeast US and significantly correlated with a poor FE (r= -0.46, p< 0.01), contrasting the mortality clusters seen in the Northeast and East North Central States (Figure 1). Soft drinks and meat/poultry consumption had a significant positive correlation with mortality (r = 0.37 and r=0.07, p< 0.01 respectively). Households in high EOCRC mortality counties consumed an average of 13.7 pounds less fruit and vegetable per year (p < 0.01). Furthermore, these counties had higher cost difference between healthy items and unhealthy equivalents, including dark leafy greens vs starchy vegetables (p < 0.01) and whole grains vs white bread (p < 0.01).
Discussion: The greatest density of EOCRC mortality is concentrated in the Southeast US, which significantly correlates with poor food environment, a modifiable risk factor. These counties had significantly reduced consumption and higher relative cost of healthy foods. Interestingly, EOCRC mortality seen in the Northeast and East North Central States do not have the same correlation with food environment, indicating a different driving factor.

Disclosures:
William K. Oelsner, MD, Arslan Kahloon, MD, Priya Vijayvargiya, MD, 6, Early Onset Colorectal Cancer Mortality Is Higher in the Southeast US and Significantly Associated With Poor Food Environment, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
William K. Oelsner, MD, Arslan Kahloon, MD, Priya Vijayvargiya, MD
University of Tennessee HSC College of Medicine Chattanooga, Chattanooga, TN
Introduction: Since the 1990s, there has been an alarming rise in the incidence and mortality of early onset colorectal cancer (EOCRC) in the US. While the exact mechanism of this rise is still unknown, there have been several proposed factors including obesity, diet, physical inactivity, and environmental exposures. The food environment (FE) is the physical, economic, and sociocultural context in which populations obtain and consume food. This is the first study to critically examine the relationship of food environments, dietary patterns, and food costs with respect to EOCRC mortality on a national level.
Methods: This national retrospective cohort study examined the county level mortality of EOCRC using data from the National Programs of Cancer Registries and Surveillance, Epidemiology and End Results Program. FE data was obtained from the Food Environment Atlas and Community Health Rankings Program. Individuals aged 20-49 residing in the contiguous US from 1999 to 2020 with colorectal cancer were included in the study. SEER*Stat was used to calculate county mortality rates; GraphPad was used to calculate Pearson correlation coefficients and unpaired t-tests with Welch correction; ArcGIS Pro was used for mapping and spatial analysis.
Results: 68,495 people from 1,307 counties met inclusion criteria. The greatest density of EOCRC mortality was concentrated in the Southeast US and significantly correlated with a poor FE (r= -0.46, p< 0.01), contrasting the mortality clusters seen in the Northeast and East North Central States (Figure 1). Soft drinks and meat/poultry consumption had a significant positive correlation with mortality (r = 0.37 and r=0.07, p< 0.01 respectively). Households in high EOCRC mortality counties consumed an average of 13.7 pounds less fruit and vegetable per year (p < 0.01). Furthermore, these counties had higher cost difference between healthy items and unhealthy equivalents, including dark leafy greens vs starchy vegetables (p < 0.01) and whole grains vs white bread (p < 0.01).
Discussion: The greatest density of EOCRC mortality is concentrated in the Southeast US, which significantly correlates with poor food environment, a modifiable risk factor. These counties had significantly reduced consumption and higher relative cost of healthy foods. Interestingly, EOCRC mortality seen in the Northeast and East North Central States do not have the same correlation with food environment, indicating a different driving factor.

Figure: Heat map demonstrating higher density of early onset colorectal cancer mortality in the Southeast US that correlates with poor food environment.
Red: Poor Food Environment and high EOCRC mortality; Purple: healthy food Environment and high EOCRC mortality; Grey: insufficient county mortality data or population to include in analysis.
Red: Poor Food Environment and high EOCRC mortality; Purple: healthy food Environment and high EOCRC mortality; Grey: insufficient county mortality data or population to include in analysis.
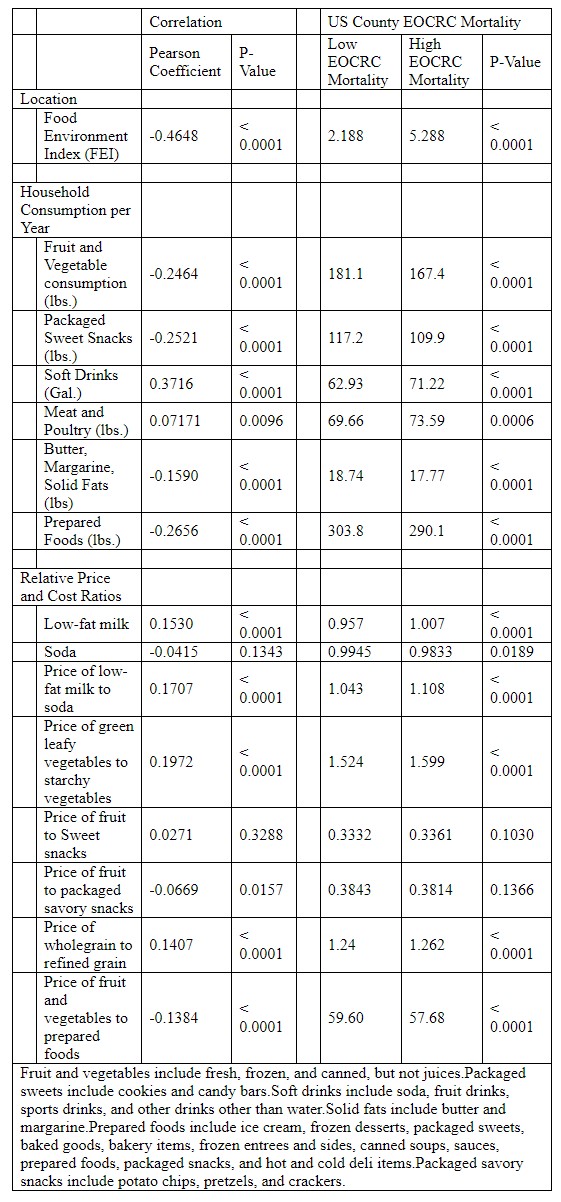
Table: Comparison of low and high EOCRC mortality counties with respect to Food Environment, household consumption, and food costs.
Disclosures:
William Oelsner indicated no relevant financial relationships.
Arslan Kahloon indicated no relevant financial relationships.
Priya Vijayvargiya indicated no relevant financial relationships.
William K. Oelsner, MD, Arslan Kahloon, MD, Priya Vijayvargiya, MD, 6, Early Onset Colorectal Cancer Mortality Is Higher in the Southeast US and Significantly Associated With Poor Food Environment, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.




