Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 4A - Biliary / Pancreas / Interventional Endoscopy
61 - Intermuscular Adipose Tissue is Associated With the Severity of Acute Pancreatitis in Hospitalized Patients
Wednesday, October 25, 2023
9:30 AM - 9:40 AM PT
Location: Ballroom A
- PC
Pedro Cortes, MD (he/him/his)
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Pedro Cortes, MD1, Tyler Mistretta, MD2, Brittany Jackson, MD1, Ahmed Salih, MD3, Caroline Olson, MD1, Panagiotis Korfiatis, PhD4, Jason Klug, PhD4, Fernando Stancampiano, MD1, Dana Harris, MD1, J Dan Echols, MD1, Rickey Carter, PhD1, Baoan Ji, MD, PhD1, Heather Hardway, PhD1, Michael Wallace, MD5, Vivek Kumbhari, MBBCh, PhD1, Yan Bi, MD, PhD1
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic Florida, Jacksonville, FL; 3Indiana University School of Medicine, Muncie, IN; 4Mayo Clinic, Rochester, MN; 5Sheikh Shakhbout Medical City, Abu Dhabi, Abu Dhabi, United Arab Emirates
Introduction: The clinical utility of body composition in predicting the severity of acute pancreatitis (AP) remains unclear. We measured body composition using artificial intelligence to describe its association with AP severity in hospitalized patients.
Methods: We performed a retrospective study of patients hospitalized with AP at three tertiary care centers in 2018. Patients with CT imaging of the abdomen at admission were included. A fully automated abdominal segmentation algorithm developed by Weston et al. (Radiology 2019) was used for body composition analysis. Figure 1. The primary outcome was severe AP, which was defined as having persistent single- or multi-organ failure as per the revised Atlanta classification. Multivariable logistic regression analysis was used.
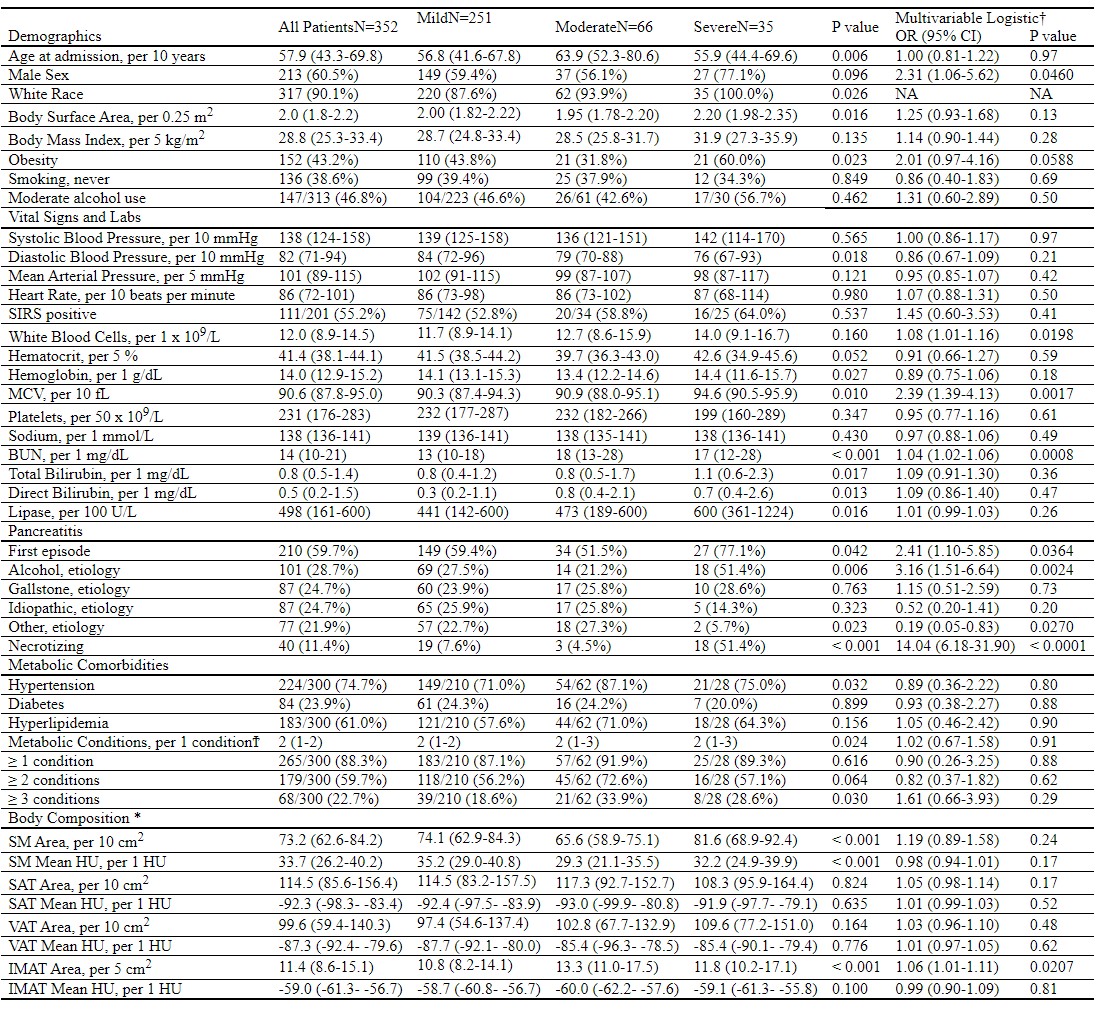
Results: 352 patients (median age 57.9 years, 60% male, 43% obesity) were included. Table 1. Severe AP occurred in 35 patients (9.9%). After adjusting for male sex and first episode of AP, only the intermuscular adipose tissue (IMAT) was significantly associated with severe AP, p = 0.0207. For every 5 cm2 increase in IMAT, there was an associated 6% increased odds of severe AP. Subcutaneous adipose tissue (SAT) approached significance, OR = 1.05, p = 0.17. Neither visceral adipose tissue (VAT) or skeletal muscle (SM) was associated with severe AP. In patients with obesity, SM was associated with severe AP at p = 0.009 in unadjusted analysis. 74 patients had pre- and admission-CT scans to compare body composition (median time between scans: 80 days, IQR: 34-114). Only the SAT had a significant change at admission, p = 0.0291, while VAT had a trend but did not reach significance, p = 0.0558. A 5% increase or decrease from baseline in SM, SAT, VAT, or IMAT on admission were not associated with the severity of AP.
Discussion: In this multi-site retrospective study, we found an elevated IMAT was associated with severe AP regardless of etiology. Although SAT was non-significant, it approached significance. Neither VAT nor SM were significant. IMAT has been reported to be strongly associated with metabolic syndrome, serum lipid levels, aging and sarcopenia. A possible mechanism may involve the pro-inflammatory effects of IMAT increasing the risk of the systemic inflammatory response syndrome in AP. Further research in larger prospective studies is needed.

1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic Florida, Jacksonville, FL; 3Indiana University School of Medicine, Muncie, IN; 4Mayo Clinic, Rochester, MN; 5Sheikh Shakhbout Medical City, Abu Dhabi, Abu Dhabi, United Arab Emirates
Introduction: The clinical utility of body composition in predicting the severity of acute pancreatitis (AP) remains unclear. We measured body composition using artificial intelligence to describe its association with AP severity in hospitalized patients.
Methods: We performed a retrospective study of patients hospitalized with AP at three tertiary care centers in 2018. Patients with CT imaging of the abdomen at admission were included. A fully automated abdominal segmentation algorithm developed by Weston et al. (Radiology 2019) was used for body composition analysis. Figure 1. The primary outcome was severe AP, which was defined as having persistent single- or multi-organ failure as per the revised Atlanta classification. Multivariable logistic regression analysis was used.
Results: 352 patients (median age 57.9 years, 60% male, 43% obesity) were included. Table 1. Severe AP occurred in 35 patients (9.9%). After adjusting for male sex and first episode of AP, only the intermuscular adipose tissue (IMAT) was significantly associated with severe AP, p = 0.0207. For every 5 cm2 increase in IMAT, there was an associated 6% increased odds of severe AP. Subcutaneous adipose tissue (SAT) approached significance, OR = 1.05, p = 0.17. Neither visceral adipose tissue (VAT) or skeletal muscle (SM) was associated with severe AP. In patients with obesity, SM was associated with severe AP at p = 0.009 in unadjusted analysis. 74 patients had pre- and admission-CT scans to compare body composition (median time between scans: 80 days, IQR: 34-114). Only the SAT had a significant change at admission, p = 0.0291, while VAT had a trend but did not reach significance, p = 0.0558. A 5% increase or decrease from baseline in SM, SAT, VAT, or IMAT on admission were not associated with the severity of AP.
Discussion: In this multi-site retrospective study, we found an elevated IMAT was associated with severe AP regardless of etiology. Although SAT was non-significant, it approached significance. Neither VAT nor SM were significant. IMAT has been reported to be strongly associated with metabolic syndrome, serum lipid levels, aging and sarcopenia. A possible mechanism may involve the pro-inflammatory effects of IMAT increasing the risk of the systemic inflammatory response syndrome in AP. Further research in larger prospective studies is needed.

Figure: Figure 1: Axial Cross-Sectional Images at L1 Vertebrae of Patients with Severe Acute Pancreatitis (AP) to Measure Body Composition. Subcutaneous Adipose Tissue (Blue), Visceral Adipose Tissue (Green), Intermuscular Adipose Tissue (Yellow) and Subcutaneous Muscle (Grey). A. Patient with normal body mass index (BMI) and necrotizing AP. B. Patient with overweight and necrotizing AP. C. Patient with class I obesity and necrotizing AP. D. Patient with class II obesity with non-necrotizing fatal AP.
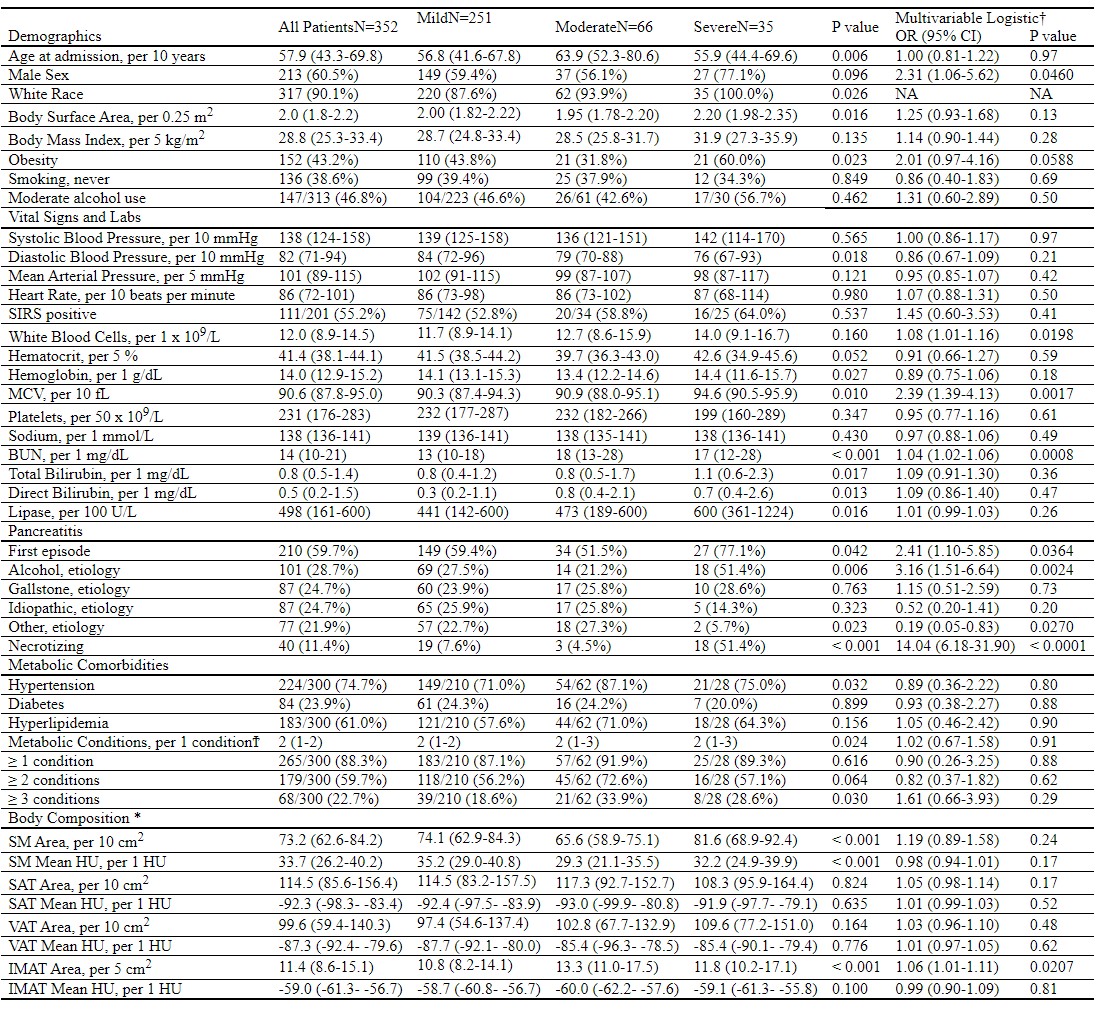
Table: Table 1: Baseline Characteristics According to Acute Pancreatitis Severity and Multivariable Logistic Regression Analysis to Predict Severe Acute Pancreatitis
OR, odd ratio, 95% CI, 95% confidence interval; SIRS, systemic inflammatory response syndrome; MCV, mean corpuscular volume; BUN, blood urea nitrogen; SM, skeletal muscle; SAT, subcutaneous adipose tissue; VAT, visceral adipose tissue; IMAT, intermuscular adipose tissue; HU, Hounsfield units.
Reference ranges: hematocrit, 38.3-48.6%, hemoglobin, 13.2-16.6 g/dL, MCV, 78.2-97.9 fL; platelets, 135 – 317 x 109 /L; sodium, 135-145 mmol/L; BUN, 8-24 mg/dL; total bilirubin, ≤ 1.2 mg/dL; direct bilirubin, 0.0-0.3 mg/dL; lipase, 13-60 U/L
Ϯ Metabolic conditions included hypertension, diabetes, or prediabetes (treated mutually exclusive), hyperlipidemia, or fatty liver. Due to the high number of missing data for fatty liver, it was not included in the analysis.
* Areas for skeletal muscle (SM), subcutaneous adipose tissue (SAT), visceral adipose tissue (VAT), and intermuscular adipose tissue (IMAT) are corrected for body surface area (BSA), calculated using the Mosteller formula. Mean HU is not corrected as it is a relative quantitative measurement of radio density, which is independent of BSA.
† Multivariable models to predict severe AP were adjusted for male sex and first episode of acute pancreatitis. The odd ratios for Male sex and first episode of acute pancreatitis in the multivariable logistic regressions were estimated using a 2-variable model constructed with those variables. The odd ratio for White Race was unable to be estimated given the zero count.
OR, odd ratio, 95% CI, 95% confidence interval; SIRS, systemic inflammatory response syndrome; MCV, mean corpuscular volume; BUN, blood urea nitrogen; SM, skeletal muscle; SAT, subcutaneous adipose tissue; VAT, visceral adipose tissue; IMAT, intermuscular adipose tissue; HU, Hounsfield units.
Reference ranges: hematocrit, 38.3-48.6%, hemoglobin, 13.2-16.6 g/dL, MCV, 78.2-97.9 fL; platelets, 135 – 317 x 109 /L; sodium, 135-145 mmol/L; BUN, 8-24 mg/dL; total bilirubin, ≤ 1.2 mg/dL; direct bilirubin, 0.0-0.3 mg/dL; lipase, 13-60 U/L
Ϯ Metabolic conditions included hypertension, diabetes, or prediabetes (treated mutually exclusive), hyperlipidemia, or fatty liver. Due to the high number of missing data for fatty liver, it was not included in the analysis.
* Areas for skeletal muscle (SM), subcutaneous adipose tissue (SAT), visceral adipose tissue (VAT), and intermuscular adipose tissue (IMAT) are corrected for body surface area (BSA), calculated using the Mosteller formula. Mean HU is not corrected as it is a relative quantitative measurement of radio density, which is independent of BSA.
† Multivariable models to predict severe AP were adjusted for male sex and first episode of acute pancreatitis. The odd ratios for Male sex and first episode of acute pancreatitis in the multivariable logistic regressions were estimated using a 2-variable model constructed with those variables. The odd ratio for White Race was unable to be estimated given the zero count.
Disclosures:
Pedro Cortes indicated no relevant financial relationships.
Tyler Mistretta indicated no relevant financial relationships.
Brittany Jackson indicated no relevant financial relationships.
Ahmed Salih indicated no relevant financial relationships.
Caroline Olson indicated no relevant financial relationships.
Panagiotis Korfiatis indicated no relevant financial relationships.
Jason Klug indicated no relevant financial relationships.
Fernando Stancampiano indicated no relevant financial relationships.
Dana Harris indicated no relevant financial relationships.
J Dan Echols indicated no relevant financial relationships.
Rickey Carter indicated no relevant financial relationships.
Baoan Ji indicated no relevant financial relationships.
Heather Hardway indicated no relevant financial relationships.
Michael Wallace indicated no relevant financial relationships.
Vivek Kumbhari indicated no relevant financial relationships.
Yan Bi indicated no relevant financial relationships.
Pedro Cortes, MD1, Tyler Mistretta, MD2, Brittany Jackson, MD1, Ahmed Salih, MD3, Caroline Olson, MD1, Panagiotis Korfiatis, PhD4, Jason Klug, PhD4, Fernando Stancampiano, MD1, Dana Harris, MD1, J Dan Echols, MD1, Rickey Carter, PhD1, Baoan Ji, MD, PhD1, Heather Hardway, PhD1, Michael Wallace, MD5, Vivek Kumbhari, MBBCh, PhD1, Yan Bi, MD, PhD1, 61, Intermuscular Adipose Tissue is Associated With the Severity of Acute Pancreatitis in Hospitalized Patients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
