Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 3A - Liver
38 - Echocardiographic Analysis of Predictors of Cardiac Dysfunction in Patients With Hereditary Hemochromatosis
Tuesday, October 24, 2023
2:25 PM - 2:35 PM PT
Location: Ballroom A
- PC
Pedro Cortes, MD (he/him/his)
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Pedro Cortes, MD, Abdelhadi Elsayed, MD, Fernando Stancampiano, MD, Fernanda Barusco, BS, Brian Shapiro, MD, Yan Bi, MD, PhD, Michael Heckman, MS, Zhongwei Peng, MS, Prakash Kempaiah, PhD, William C. Palmer, MD
Mayo Clinic, Jacksonville, FL
Introduction: Hereditary hemochromatosis (HH) is a heterogenous genetic disorder of excess body iron storages caused by unregulated intestinal iron absorption. Approximately 15% of patients with HH have cardiac involvement with 0.9 to 3.0% classically developing an infiltrative, restrictive cardiomyopathy. We described the correlation between echocardiographic findings and cardiac dysfunction in patients with HH.
Methods: In this retrospective study, we included patients with HH who underwent transthoracic echocardiography at a tertiary care center between August 2000 and July 2022. We defined three primary outcomes for cardiac dysfunction: 1) left ventricular ejection fraction (LVEF) < 55 %, 2) ratio between early mitral inflow velocity and mitral annular early diastolic velocity (E/e’) > 15, and 3) global longitudinal strain (GLS) > -18. Multivariable logistic regression was used to identify predictors for cardiac dysfunction.
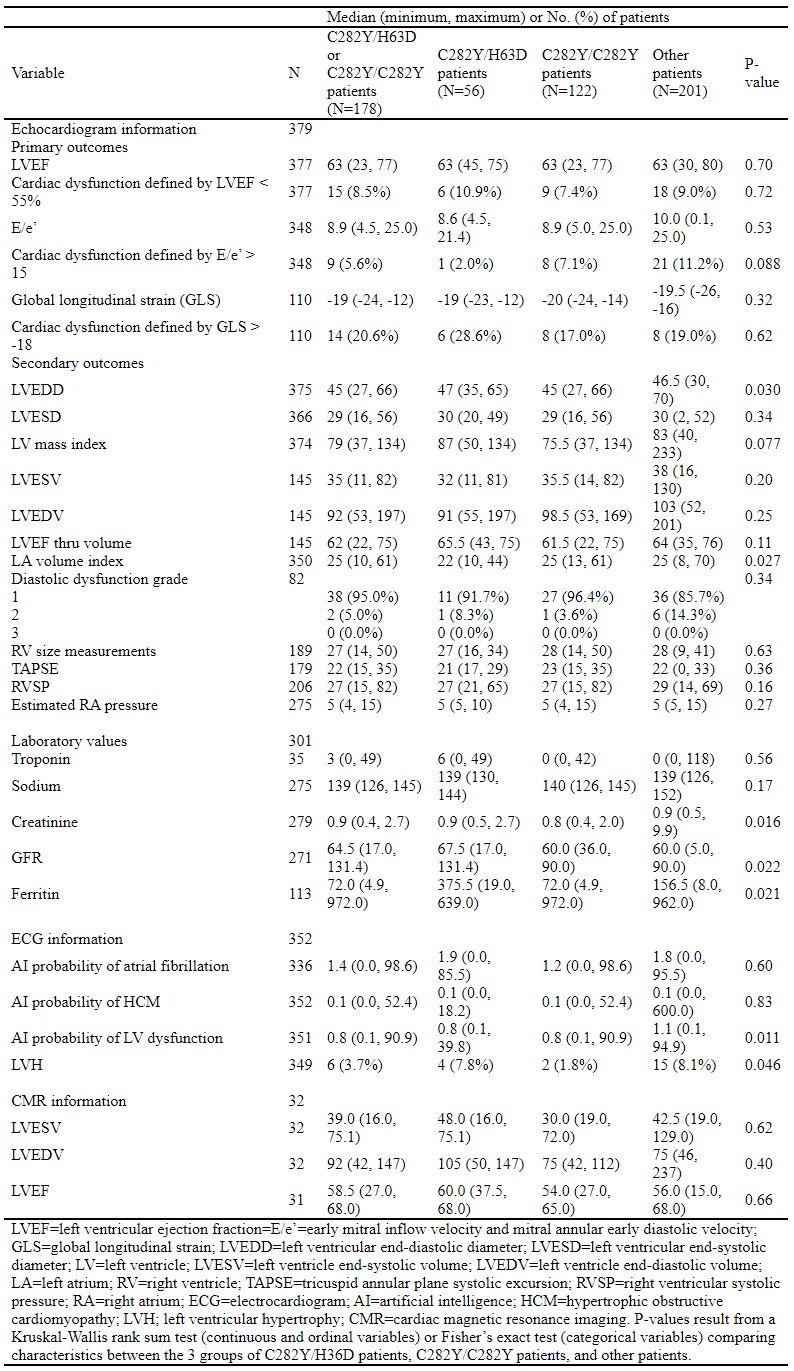
Results: 582 patients (median age 57 years, 61.2% male) were included. The frequency of LVEF < 55%, E/e’ > 15 and GLS > -18 were 9.0% (52/580), 9.6% (51/534) and 20.2% (25/124), respectively. Table 1. In multivariable analysis, non-White race (OR 4.36, p=0.007), and C282Y/H36D genetic mutation (OR 0.10, p=0.034) were associated with E/e’ > 15. No specific HFE genetic mutation was associated with LVEF < 55%. A history of myocardial infarction was strongly associated with both LVEF < 55% and E/e’ > 15. Patients with C282Y/H63D had a higher frequency of myocardial infarction. Smoking and alcohol use were significantly associated with GLS > -18 in unadjusted analysis.
Discussion: To our knowledge, this is the largest study to summarize the echocardiographic findings in patients with HH and the only to determine risk factors and the effects of HFE genetic mutations on cardiac dysfunction. We found the traditional risk factors of male sex, and history of myocardial infarction or heart failure, were associated with a reduced LVEF, irrespective of the underlying HFE genetic mutation. We found patients with a C282Y/H63D genetic mutation had a higher frequency of myocardial infarction, yet this mutation was associated with reduced odds of diastolic dysfunction compared to other genetic mutations. Our findings reinforce the usefulness of echocardiography as a screening test in HH. A potential application of our findings is the derivation of a risk score to predict cardiac dysfunction in patients with HH.

Disclosures:
Pedro Cortes, MD, Abdelhadi Elsayed, MD, Fernando Stancampiano, MD, Fernanda Barusco, BS, Brian Shapiro, MD, Yan Bi, MD, PhD, Michael Heckman, MS, Zhongwei Peng, MS, Prakash Kempaiah, PhD, William C. Palmer, MD, 38, Echocardiographic Analysis of Predictors of Cardiac Dysfunction in Patients With Hereditary Hemochromatosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Mayo Clinic, Jacksonville, FL
Introduction: Hereditary hemochromatosis (HH) is a heterogenous genetic disorder of excess body iron storages caused by unregulated intestinal iron absorption. Approximately 15% of patients with HH have cardiac involvement with 0.9 to 3.0% classically developing an infiltrative, restrictive cardiomyopathy. We described the correlation between echocardiographic findings and cardiac dysfunction in patients with HH.
Methods: In this retrospective study, we included patients with HH who underwent transthoracic echocardiography at a tertiary care center between August 2000 and July 2022. We defined three primary outcomes for cardiac dysfunction: 1) left ventricular ejection fraction (LVEF) < 55 %, 2) ratio between early mitral inflow velocity and mitral annular early diastolic velocity (E/e’) > 15, and 3) global longitudinal strain (GLS) > -18. Multivariable logistic regression was used to identify predictors for cardiac dysfunction.
Results: 582 patients (median age 57 years, 61.2% male) were included. The frequency of LVEF < 55%, E/e’ > 15 and GLS > -18 were 9.0% (52/580), 9.6% (51/534) and 20.2% (25/124), respectively. Table 1. In multivariable analysis, non-White race (OR 4.36, p=0.007), and C282Y/H36D genetic mutation (OR 0.10, p=0.034) were associated with E/e’ > 15. No specific HFE genetic mutation was associated with LVEF < 55%. A history of myocardial infarction was strongly associated with both LVEF < 55% and E/e’ > 15. Patients with C282Y/H63D had a higher frequency of myocardial infarction. Smoking and alcohol use were significantly associated with GLS > -18 in unadjusted analysis.
Discussion: To our knowledge, this is the largest study to summarize the echocardiographic findings in patients with HH and the only to determine risk factors and the effects of HFE genetic mutations on cardiac dysfunction. We found the traditional risk factors of male sex, and history of myocardial infarction or heart failure, were associated with a reduced LVEF, irrespective of the underlying HFE genetic mutation. We found patients with a C282Y/H63D genetic mutation had a higher frequency of myocardial infarction, yet this mutation was associated with reduced odds of diastolic dysfunction compared to other genetic mutations. Our findings reinforce the usefulness of echocardiography as a screening test in HH. A potential application of our findings is the derivation of a risk score to predict cardiac dysfunction in patients with HH.

Figure: Figure 1: Transthoracic Echocardiography of Reduced Left Ventricular Ejection Fraction. Panels A and D show diastole and Panels B and C shows systole. Panels A and C show the apical four chamber view. Panels B and D show the parasternal long axis. LV, left ventricle, RV, right ventricle.
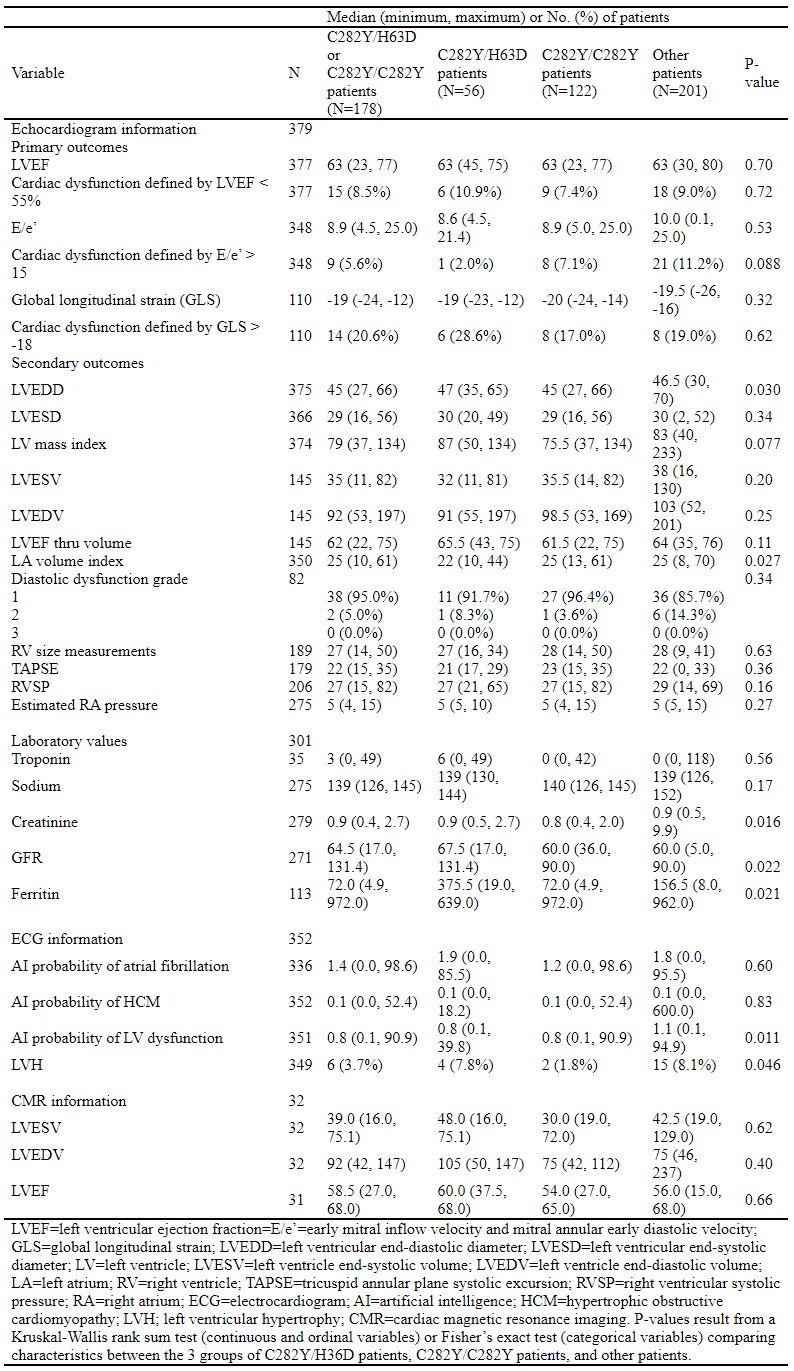
Table: Table 1: Comparison of echocardiogram, laboratory, ECG, and CMR information according to HFE genetics
Disclosures:
Pedro Cortes indicated no relevant financial relationships.
Abdelhadi Elsayed indicated no relevant financial relationships.
Fernando Stancampiano indicated no relevant financial relationships.
Fernanda Barusco indicated no relevant financial relationships.
Brian Shapiro indicated no relevant financial relationships.
Yan Bi indicated no relevant financial relationships.
Michael Heckman indicated no relevant financial relationships.
Zhongwei Peng indicated no relevant financial relationships.
Prakash Kempaiah indicated no relevant financial relationships.
William Palmer indicated no relevant financial relationships.
Pedro Cortes, MD, Abdelhadi Elsayed, MD, Fernando Stancampiano, MD, Fernanda Barusco, BS, Brian Shapiro, MD, Yan Bi, MD, PhD, Michael Heckman, MS, Zhongwei Peng, MS, Prakash Kempaiah, PhD, William C. Palmer, MD, 38, Echocardiographic Analysis of Predictors of Cardiac Dysfunction in Patients With Hereditary Hemochromatosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
