Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 2A - Functional / Esophagus
26 - COuGH RefluX: Externally Validated Risk Prediction Score for Laryngopharyngeal Reflux Symptoms
Tuesday, October 24, 2023
9:40 AM - 9:50 AM PT
Location: Ballroom A

Amanda J. Krause, MD (she/her/hers)
University of California San Diego
La Jolla, CA
Presenting Author(s)
Award: Outstanding Research Award in the Esophagus Category (Trainee)
Amanda J. Krause, MD1, Alexander Kaizer, PhD2, Dustin Carlson, MD, MS3, Walter W. Chan, MD, MPH4, Chien-Lin Chen, MD, PhD5, C. Prakash Gyawali, MD, MRCP6, Andrew Jenkins, MD4, John E. Pandolfino, MD, MSCI, FACG3, Vinathi Polamraju, MD7, Ming-Wun Wong, MD, PhD5, Maddi Greytak, BA8, Rena Yadlapati, MD, MS9
1University of California San Diego, La Jolla, CA; 2University of Colorado Anschutz Medical Campus, Aurora, CO; 3Northwestern University Feinberg School of Medicine, Chicago, IL; 4Brigham and Women's Hospital, Boston, MA; 5Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation and Tzu Chi University, Hualien, Hualien, Taiwan; 6Washington University School of Medicine, St. Louis, MO; 7Washington University in St. Louis, St. Louis, MO; 8UC San Diego Health, La Jolla, CA; 9University of California San Diego, San Diego, CA
Introduction: Discerning whether laryngeal symptoms result from gastroesophageal reflux (GER) is critically challenging in making a conclusive diagnoses of laryngopharyngeal reflux (LPR), often leading to multiple tests, treatments and poor outcomes. A reliable clinical tool to stratify likelihood of LPR is needed. Thus, this study aimed to develop and validate a clinically practical risk prediction model for LPR symptoms.
Methods: This two-phase international multicenter (4 North American & 1 Asian centers) study included adults with chronic laryngeal symptoms (throat clearing, sore throat, dysphonia, cough, globus). Patients were categorized as LPR+ or LPR- based on presence or absence of: Los Angeles B/C/D esophagitis and/or long segment Barrett’s esophagus on endoscopy, acid exposure time (AET) ≥ 6% and/or ≥ 80 reflux events/24h on ambulatory reflux monitoring off PPI, or AET ≥ 2% and/or ≥ 40 reflux events on 24h impedance-pH on PPI.
First, clinical and demographic data from a single center training cohort informed models to predict LPR+. Among multiple logistic regression models an optimal model was discriminated by receiver operating characteristic curves. Beta coefficients informed a weighted model with an a priori goal to identify a lower threshold with < 20% false negative rate and upper threshold with < 20% false positive rate. Next, areas under the curve (AUC) of the weighted model were assessed among a validation cohort across five sites [R v4.2.0 (Vienna, Austria)].
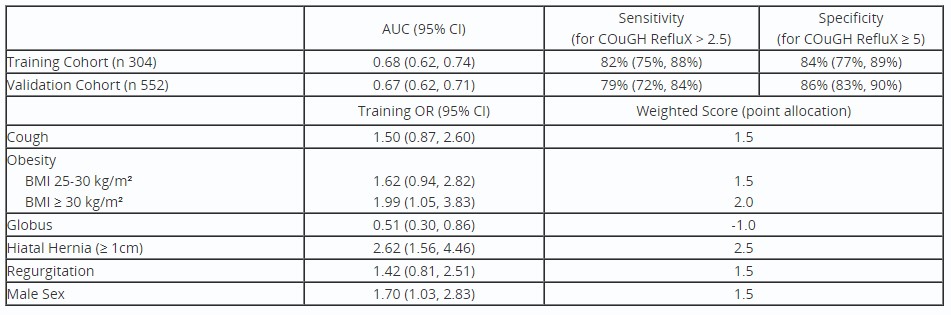
Results: A total of 856 patients were included: 304 in training cohort and 552 in validation cohort. Among the training cohort, the optimal predictive model [AUC 0.69 (95% CI 0.63, 0.75)] consisted of Cough, Overweight/obesity, Globus, Hiatal Hernia ≥ 1cm, Regurgitation, and seX (Male) (Table). The weighted COuGH RefluX with lower threshold of 2.5 and upper threshold of 5 was 82% sensitive and 84% specific for LPR. Among the validation cohort, the AUC for the weighted COuGH RefluX was 0.67 (0.62, 0.71) with 79% sensitivity and 86% specificity for LPR (Figure).
Discussion: The externally validated COuGH RefluX score is a clinically practical model to predict likelihood of LPR. The score classifies most patients with chronic laryngeal symptoms as low/high likelihood of LPR, and only 38% as indeterminate, who would require further evaluation. Thus, the COuGH RefluX can guide diagnostic/therapeutic strategies, and reduce inappropriate PPI use/testing for patients referred for LPR evaluation.

Disclosures:
Amanda J. Krause, MD1, Alexander Kaizer, PhD2, Dustin Carlson, MD, MS3, Walter W. Chan, MD, MPH4, Chien-Lin Chen, MD, PhD5, C. Prakash Gyawali, MD, MRCP6, Andrew Jenkins, MD4, John E. Pandolfino, MD, MSCI, FACG3, Vinathi Polamraju, MD7, Ming-Wun Wong, MD, PhD5, Maddi Greytak, BA8, Rena Yadlapati, MD, MS9, 26, COuGH RefluX: Externally Validated Risk Prediction Score for Laryngopharyngeal Reflux Symptoms, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Amanda J. Krause, MD1, Alexander Kaizer, PhD2, Dustin Carlson, MD, MS3, Walter W. Chan, MD, MPH4, Chien-Lin Chen, MD, PhD5, C. Prakash Gyawali, MD, MRCP6, Andrew Jenkins, MD4, John E. Pandolfino, MD, MSCI, FACG3, Vinathi Polamraju, MD7, Ming-Wun Wong, MD, PhD5, Maddi Greytak, BA8, Rena Yadlapati, MD, MS9
1University of California San Diego, La Jolla, CA; 2University of Colorado Anschutz Medical Campus, Aurora, CO; 3Northwestern University Feinberg School of Medicine, Chicago, IL; 4Brigham and Women's Hospital, Boston, MA; 5Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation and Tzu Chi University, Hualien, Hualien, Taiwan; 6Washington University School of Medicine, St. Louis, MO; 7Washington University in St. Louis, St. Louis, MO; 8UC San Diego Health, La Jolla, CA; 9University of California San Diego, San Diego, CA
Introduction: Discerning whether laryngeal symptoms result from gastroesophageal reflux (GER) is critically challenging in making a conclusive diagnoses of laryngopharyngeal reflux (LPR), often leading to multiple tests, treatments and poor outcomes. A reliable clinical tool to stratify likelihood of LPR is needed. Thus, this study aimed to develop and validate a clinically practical risk prediction model for LPR symptoms.
Methods: This two-phase international multicenter (4 North American & 1 Asian centers) study included adults with chronic laryngeal symptoms (throat clearing, sore throat, dysphonia, cough, globus). Patients were categorized as LPR+ or LPR- based on presence or absence of: Los Angeles B/C/D esophagitis and/or long segment Barrett’s esophagus on endoscopy, acid exposure time (AET) ≥ 6% and/or ≥ 80 reflux events/24h on ambulatory reflux monitoring off PPI, or AET ≥ 2% and/or ≥ 40 reflux events on 24h impedance-pH on PPI.
First, clinical and demographic data from a single center training cohort informed models to predict LPR+. Among multiple logistic regression models an optimal model was discriminated by receiver operating characteristic curves. Beta coefficients informed a weighted model with an a priori goal to identify a lower threshold with < 20% false negative rate and upper threshold with < 20% false positive rate. Next, areas under the curve (AUC) of the weighted model were assessed among a validation cohort across five sites [R v4.2.0 (Vienna, Austria)].
Results: A total of 856 patients were included: 304 in training cohort and 552 in validation cohort. Among the training cohort, the optimal predictive model [AUC 0.69 (95% CI 0.63, 0.75)] consisted of Cough, Overweight/obesity, Globus, Hiatal Hernia ≥ 1cm, Regurgitation, and seX (Male) (Table). The weighted COuGH RefluX with lower threshold of 2.5 and upper threshold of 5 was 82% sensitive and 84% specific for LPR. Among the validation cohort, the AUC for the weighted COuGH RefluX was 0.67 (0.62, 0.71) with 79% sensitivity and 86% specificity for LPR (Figure).
Discussion: The externally validated COuGH RefluX score is a clinically practical model to predict likelihood of LPR. The score classifies most patients with chronic laryngeal symptoms as low/high likelihood of LPR, and only 38% as indeterminate, who would require further evaluation. Thus, the COuGH RefluX can guide diagnostic/therapeutic strategies, and reduce inappropriate PPI use/testing for patients referred for LPR evaluation.

Figure: Figure: Receiver operating characteristics of validation cohort
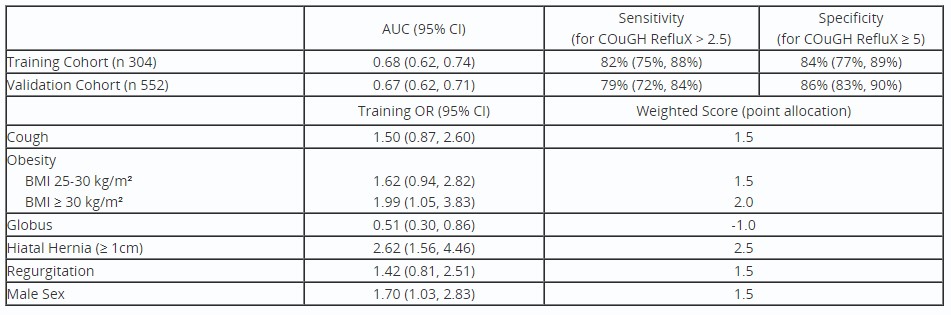
Table: Table: Model Results
Disclosures:
Amanda Krause indicated no relevant financial relationships.
Alexander Kaizer indicated no relevant financial relationships.
Dustin Carlson: Braintree Pharmaceuticals – Consultant. Medtronic, Inc – Consultant, Intellectual Property/Patents, Speakers Bureau. Phathom Pharmaceuticals – Advisory Committee/Board Member.
Walter Chan: Phathom Pharmaceutical – Advisory Committee/Board Member. Regeneron Pharmaceutical – Advisory Committee/Board Member. Sanofi Pharmaceutical – Advisory Committee/Board Member.
Chien-Lin Chen indicated no relevant financial relationships.
C. Prakash Gyawali: Diversatek – Consultant, Grant/Research Support. Medtronic – Consultant.
Andrew Jenkins indicated no relevant financial relationships.
John Pandolfino: AlfaSigma – Consultant. endogastric solutions – Consultant, Speakers Bureau. Ethicon/ J&J – Advisory Committee/Board Member, Consultant, Speakers Bureau. Medtronic – Advisor or Review Panel Member, Consultant, Intellectual Property/Patents, Royalties, Speakers Bureau. Phathom – Consultant. Takeda – Consultant, Speakers Bureau.
Vinathi Polamraju indicated no relevant financial relationships.
Ming-Wun Wong indicated no relevant financial relationships.
Maddi Greytak indicated no relevant financial relationships.
Rena Yadlapati: Ironwood – Grant/Research Support. Medscape – Consultant. Medtronic – Consultant. Phathom – Consultant. Reckitt Benckiser Healthcare Ltd – Consultant. RJS Mediagnostix – Advisory Committee/Board Member, Stock Options. StatLinkMD – Consultant.
Amanda J. Krause, MD1, Alexander Kaizer, PhD2, Dustin Carlson, MD, MS3, Walter W. Chan, MD, MPH4, Chien-Lin Chen, MD, PhD5, C. Prakash Gyawali, MD, MRCP6, Andrew Jenkins, MD4, John E. Pandolfino, MD, MSCI, FACG3, Vinathi Polamraju, MD7, Ming-Wun Wong, MD, PhD5, Maddi Greytak, BA8, Rena Yadlapati, MD, MS9, 26, COuGH RefluX: Externally Validated Risk Prediction Score for Laryngopharyngeal Reflux Symptoms, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

