Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 2A - Functional / Esophagus
23 - Upper GI Endoscopy With Ambulatory Reflux Monitoring and Trialing PPI Discontinuation Optimizes Cost Effectiveness to Manage Heartburn
Tuesday, October 24, 2023
9:10 AM - 9:20 AM PT
Location: Ballroom A
.jpg)
Eric D. Shah, MD, MBA, FACG
University of Michigan
Ann Arbor, MI
Presenting Author(s)
Eric D. Shah, MD, MBA, FACG1, Walter W. Chan, MD, MPH2, Daniela Jodorkovsky, MD3, Kristle Lee Lynch, MD4, Amit Patel, MD5, Dhyanesh Patel, MD6, Rena Yadlapati, MD, MS7
1University of Michigan, Ann Arbor, MI; 2Brigham and Women's Hospital, Boston, MA; 3Mount Sinai, New York, NY; 4University of Pennsylvania, Philadelphia, PA; 5Duke University, Durham, NC; 6Vanderbilt University Medical Center, Nashville, TN; 7University of California San Diego, San Diego, CA
Introduction: Heartburn is a classic GERD symptom that drives many gastroenterology referrals. Recent ACG guidelines advocate ambulatory reflux monitoring when patients fail PPI therapy, but such care is rarely offered due to concerns of cost and necessity. Further controversy exists between PPI optimization vs. discontinuation when erosive findings are absent. We performed an economic analysis comparing several strategies for the management of PPI non-responsive heartburn.
Methods: A Markov model compared four strategies to manage patients with heartburn failing empiric PPI therapy and without alarm features: (1) Reassurance without testing; (2) EGD with trial of PPI optimization; (3) EGD with trial of PPI discontinuation when erosive findings are absent; (4) EGD with ambulatory reflux monitoring and trial of PPI discontinuation to phenotype subsequent care. Model inputs were defined on systematic reviews and trials linking diagnostic testing to clinical outcomes with subsequent management strategies and national cost databases. Our time horizon was 1 year with a willingness-to-pay threshold of $100,000/quality-adjusted-life-year (QALY) gained.
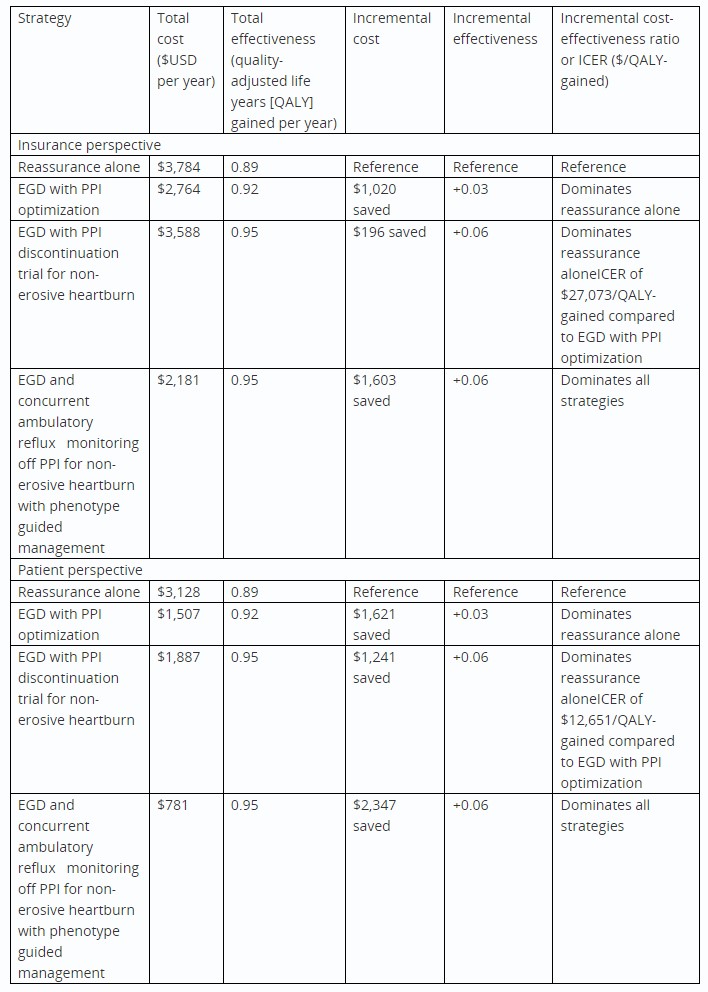
Results: From the insurance perspective, the cost of reassurance without testing (Strategy 1) was $3,784/year. EGD with PPI optimization (Strategy 2) reduced insurance costs and added health gains by optimizing management of erosive disease and non-erosive GERD. EGD with PPI discontinuation when erosive findings are absent (Strategy 3) increased costs by $813 compared to offering PPI optimization, because PPI discontinuation delayed symptom relief for many patients. However, PPI discontinuation was more cost-effective by identifying patients that did not need PPI. From the patient perspective, reassurance without testing cost $3,128/year due to out-of-pocket healthcare expenses and lower work productivity. By phenotyping management on physiology, EGD with ambulatory reflux monitoring and a trial of PPI discontinuation (Strategy 4) was the least expensive strategy (saving $1,603 to insurance and $2,347 to patients compared to reassurance without testing) and generated the greatest health gains (+0.06 QALY gain or 22 additional healthy days per year).
Discussion: EGD with ambulatory reflux monitoring performed OFF-PPI optimizes cost-effective care for patients that seek gastroenterologist advice for heartburn failing empiric PPI. When erosive findings are absent, trialing PPI discontinuation is a more cost-effective best next step than trialing PPI optimization.

Disclosures:
Eric D. Shah, MD, MBA, FACG1, Walter W. Chan, MD, MPH2, Daniela Jodorkovsky, MD3, Kristle Lee Lynch, MD4, Amit Patel, MD5, Dhyanesh Patel, MD6, Rena Yadlapati, MD, MS7, 23, Upper GI Endoscopy With Ambulatory Reflux Monitoring and Trialing PPI Discontinuation Optimizes Cost Effectiveness to Manage Heartburn, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Michigan, Ann Arbor, MI; 2Brigham and Women's Hospital, Boston, MA; 3Mount Sinai, New York, NY; 4University of Pennsylvania, Philadelphia, PA; 5Duke University, Durham, NC; 6Vanderbilt University Medical Center, Nashville, TN; 7University of California San Diego, San Diego, CA
Introduction: Heartburn is a classic GERD symptom that drives many gastroenterology referrals. Recent ACG guidelines advocate ambulatory reflux monitoring when patients fail PPI therapy, but such care is rarely offered due to concerns of cost and necessity. Further controversy exists between PPI optimization vs. discontinuation when erosive findings are absent. We performed an economic analysis comparing several strategies for the management of PPI non-responsive heartburn.
Methods: A Markov model compared four strategies to manage patients with heartburn failing empiric PPI therapy and without alarm features: (1) Reassurance without testing; (2) EGD with trial of PPI optimization; (3) EGD with trial of PPI discontinuation when erosive findings are absent; (4) EGD with ambulatory reflux monitoring and trial of PPI discontinuation to phenotype subsequent care. Model inputs were defined on systematic reviews and trials linking diagnostic testing to clinical outcomes with subsequent management strategies and national cost databases. Our time horizon was 1 year with a willingness-to-pay threshold of $100,000/quality-adjusted-life-year (QALY) gained.
Results: From the insurance perspective, the cost of reassurance without testing (Strategy 1) was $3,784/year. EGD with PPI optimization (Strategy 2) reduced insurance costs and added health gains by optimizing management of erosive disease and non-erosive GERD. EGD with PPI discontinuation when erosive findings are absent (Strategy 3) increased costs by $813 compared to offering PPI optimization, because PPI discontinuation delayed symptom relief for many patients. However, PPI discontinuation was more cost-effective by identifying patients that did not need PPI. From the patient perspective, reassurance without testing cost $3,128/year due to out-of-pocket healthcare expenses and lower work productivity. By phenotyping management on physiology, EGD with ambulatory reflux monitoring and a trial of PPI discontinuation (Strategy 4) was the least expensive strategy (saving $1,603 to insurance and $2,347 to patients compared to reassurance without testing) and generated the greatest health gains (+0.06 QALY gain or 22 additional healthy days per year).
Discussion: EGD with ambulatory reflux monitoring performed OFF-PPI optimizes cost-effective care for patients that seek gastroenterologist advice for heartburn failing empiric PPI. When erosive findings are absent, trialing PPI discontinuation is a more cost-effective best next step than trialing PPI optimization.

Figure: FIGURE: From an insurance perspective, sensitivity analysis demonstrates that up-front costs of diagnostic testing are outweighed by reductions in downstream healthcare utilization and greater health gains, when upper endoscopy (EGD) with ambulatory reflux monitoring is performed.
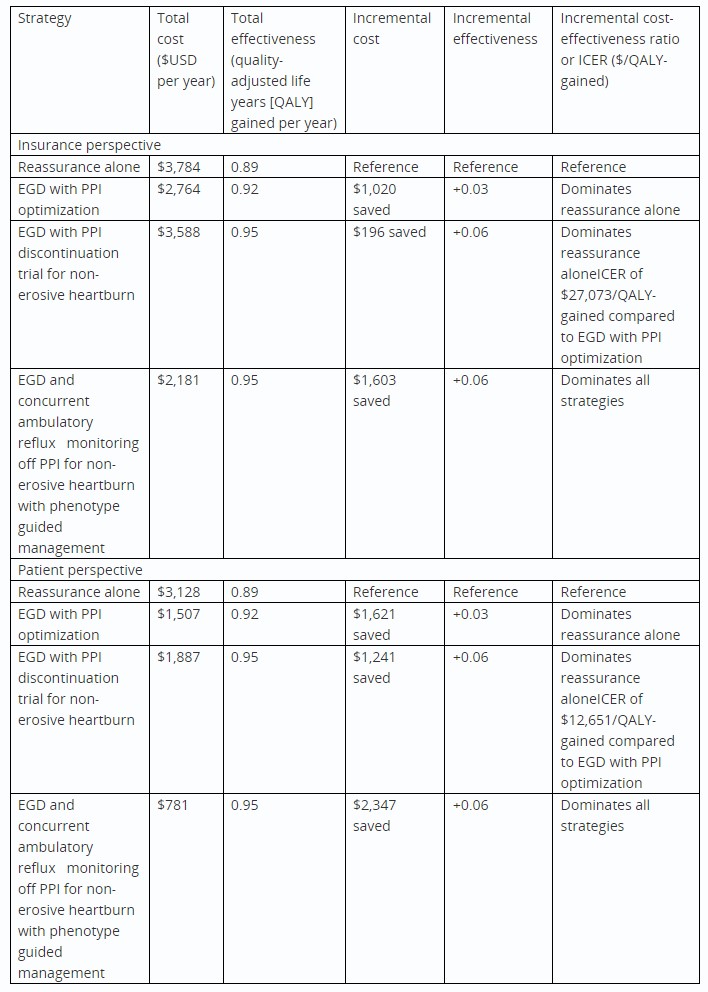
Table: TABLE: Cost-effectiveness of management algorithms for heartburn failing an empiric PPI trial in general gastroenterology
Disclosures:
Eric Shah: Ardelyx – Advisory Committee/Board Member, Consultant. GI Supply/Laborie – Advisory Committee/Board Member, Consultant. Mahana – Consultant. Neuraxis – Consultant. Salix – Advisory Committee/Board Member. Sanofi – Advisory Committee/Board Member, Consultant. Takeda – Consultant.
Walter Chan: Phathom Pharmaceutical – Advisory Committee/Board Member. Regeneron Pharmaceutical – Advisory Committee/Board Member. Sanofi Pharmaceutical – Advisory Committee/Board Member.
Daniela Jodorkovsky: ATMO Biosciences – Consultant.
Kristle Lee Lynch: Medtronic – Consultant.
Amit Patel: Medpace – Consultant. Renexxion – Consultant.
Dhyanesh Patel indicated no relevant financial relationships.
Rena Yadlapati: Ironwood – Grant/Research Support. Medscape – Consultant. Medtronic – Consultant. Phathom – Consultant. Reckitt Benckiser Healthcare Ltd – Consultant. RJS Mediagnostix – Advisory Committee/Board Member, Stock Options. StatLinkMD – Consultant.
Eric D. Shah, MD, MBA, FACG1, Walter W. Chan, MD, MPH2, Daniela Jodorkovsky, MD3, Kristle Lee Lynch, MD4, Amit Patel, MD5, Dhyanesh Patel, MD6, Rena Yadlapati, MD, MS7, 23, Upper GI Endoscopy With Ambulatory Reflux Monitoring and Trialing PPI Discontinuation Optimizes Cost Effectiveness to Manage Heartburn, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
