Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 2B - Small Intestine / IBD
30 - The Effect of Low-Dose Aspirin on Disease Activity in Pregnant Individuals with Inflammatory Bowel Disease
Tuesday, October 24, 2023
8:50 AM - 9:00 AM PT
Location: Ballroom B
.jpg)
Uma Mahadevan, MD, FACG
Professor of Clinical Medicine, Director
University of California
San Francisco, California
Presenting Author(s)
Amy Yu, MD1, Cynthia L. Fenton, MD1, Timothy Wen, MD2, Roxanna A. Irani, MD, PhD2, Uma Mahadevan, MD2
1University of California, San Francisco, San Francisco, CA; 2University of California San Francisco, San Francisco, CA
Introduction: Low-dose aspirin (LDA) prophylaxis is recommended for prevention of hypertensive disorders of pregnancy (HDP, including eclampsia, preeclampsia and gestational hypertension) in pregnant individuals at elevated risk. However, regular nonsteroidal anti-inflammatory drug use raises concerns of increased disease activity in patients with inflammatory bowel disease (IBD). We aimed to evaluate the prevalence of LDA use in pregnant IBD patients and the effect of LDA on IBD disease activity.
Methods: All individuals with IBD and at least one pregnancy followed by the Maternal Fetal Medicine (MFM) clinic between 1/2013 and 12/2022 at a tertiary academic center were included. We noted date and dose of LDA use, if prescribed. IBD outcomes included disease flare during pregnancy or six-months postpartum, defined as IBD-related hospitalization/surgery, new therapy initiation, elevated fecal calprotectin, or new active endoscopic disease. Predictors of outcomes were explored using univariable and multivariable logistic regression.
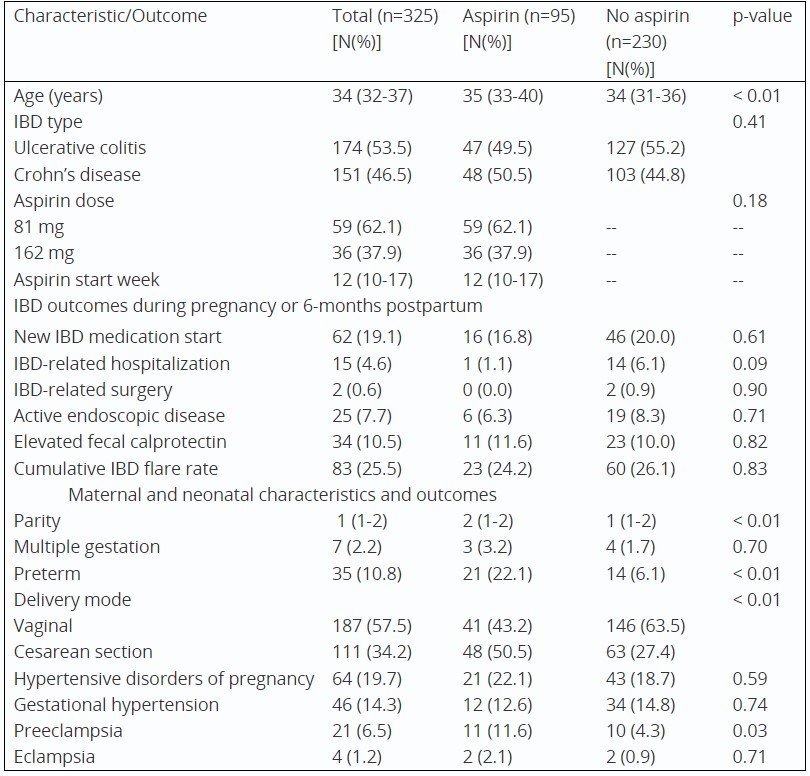
Results: Among 325 patients, the median age at time of pregnancy was 34 years, with 53% and 47% having ulcerative colitis (UC) and Crohn’s disease respectively. Ninety-five patients (29%) used LDA while 230 (71%) did not during pregnancy. There was no significant difference in prior IBD medication use or baseline disease distribution or extent; however, patients who used LDA were older than those who did not use LDA (35 vs 34 median years, p< 0.01). The cumulative rate of IBD flare during pregnancy or postpartum was similar among those who took LDA and those who did not (24% vs 26%, p=0.83). Individuals on LDA were more likely to have preterm birth (21% vs 14%), higher parity (2 vs 1), and cesarean delivery (51% vs 27%) than individuals not on LDA, (all p< 0.01). Both groups had similar cumulative rates of HDP (22% vs 19%, p=0.59), though individuals on LDA had higher rates of preeclampsia than those not on LDA (11.6% vs 4.3%, p=0.03) (Table 1). In univariable logistic regression, higher LDA dose of 162 mg (OR 2.77, 95%CI 1.07-7.41) and diagnosis of UC (OR 2.34, 95%CI 1.39-4.02) were associated with flare, with the diagnosis of UC remaining significant after adjusting for LDA dose and prior IBD medication use (OR 4.49, 95%CI 1.56-14.79).
Discussion: Approximately one-third of patients with IBD cared for in a MFM practice used LDA for prevention of HDP. Overall, the use of LDA among pregnant women with IBD was not associated with an increased risk of disease activity.
Disclosures:
Amy Yu, MD1, Cynthia L. Fenton, MD1, Timothy Wen, MD2, Roxanna A. Irani, MD, PhD2, Uma Mahadevan, MD2, 30, The Effect of Low-Dose Aspirin on Disease Activity in Pregnant Individuals with Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of California, San Francisco, San Francisco, CA; 2University of California San Francisco, San Francisco, CA
Introduction: Low-dose aspirin (LDA) prophylaxis is recommended for prevention of hypertensive disorders of pregnancy (HDP, including eclampsia, preeclampsia and gestational hypertension) in pregnant individuals at elevated risk. However, regular nonsteroidal anti-inflammatory drug use raises concerns of increased disease activity in patients with inflammatory bowel disease (IBD). We aimed to evaluate the prevalence of LDA use in pregnant IBD patients and the effect of LDA on IBD disease activity.
Methods: All individuals with IBD and at least one pregnancy followed by the Maternal Fetal Medicine (MFM) clinic between 1/2013 and 12/2022 at a tertiary academic center were included. We noted date and dose of LDA use, if prescribed. IBD outcomes included disease flare during pregnancy or six-months postpartum, defined as IBD-related hospitalization/surgery, new therapy initiation, elevated fecal calprotectin, or new active endoscopic disease. Predictors of outcomes were explored using univariable and multivariable logistic regression.
Results: Among 325 patients, the median age at time of pregnancy was 34 years, with 53% and 47% having ulcerative colitis (UC) and Crohn’s disease respectively. Ninety-five patients (29%) used LDA while 230 (71%) did not during pregnancy. There was no significant difference in prior IBD medication use or baseline disease distribution or extent; however, patients who used LDA were older than those who did not use LDA (35 vs 34 median years, p< 0.01). The cumulative rate of IBD flare during pregnancy or postpartum was similar among those who took LDA and those who did not (24% vs 26%, p=0.83). Individuals on LDA were more likely to have preterm birth (21% vs 14%), higher parity (2 vs 1), and cesarean delivery (51% vs 27%) than individuals not on LDA, (all p< 0.01). Both groups had similar cumulative rates of HDP (22% vs 19%, p=0.59), though individuals on LDA had higher rates of preeclampsia than those not on LDA (11.6% vs 4.3%, p=0.03) (Table 1). In univariable logistic regression, higher LDA dose of 162 mg (OR 2.77, 95%CI 1.07-7.41) and diagnosis of UC (OR 2.34, 95%CI 1.39-4.02) were associated with flare, with the diagnosis of UC remaining significant after adjusting for LDA dose and prior IBD medication use (OR 4.49, 95%CI 1.56-14.79).
Discussion: Approximately one-third of patients with IBD cared for in a MFM practice used LDA for prevention of HDP. Overall, the use of LDA among pregnant women with IBD was not associated with an increased risk of disease activity.
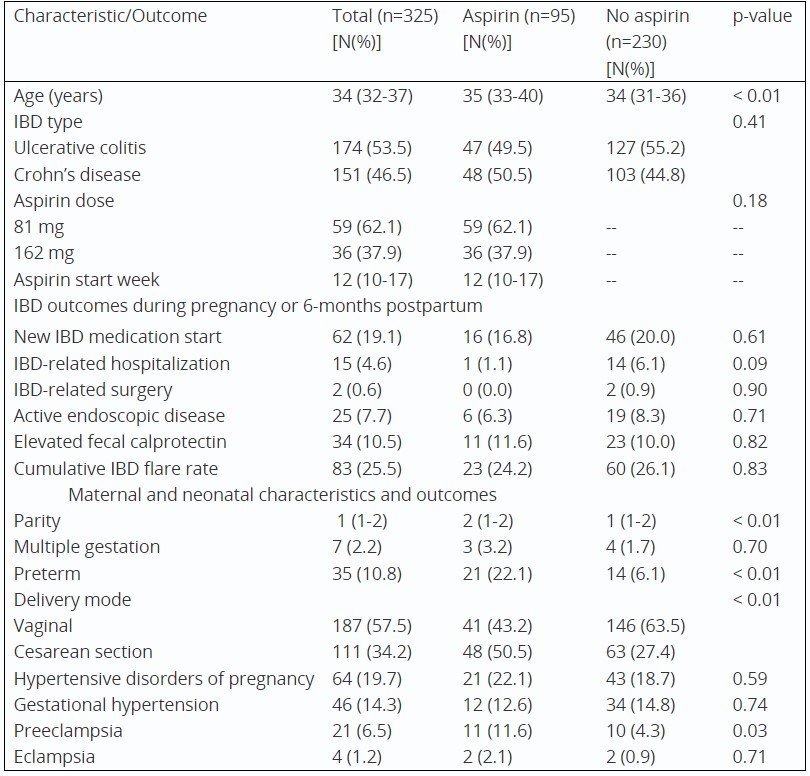
Table: Values reported as number (percentage) or median (interquartile range); Abbreviations: IBD, inflammatory bowel disease
Disclosures:
Amy Yu indicated no relevant financial relationships.
Cynthia Fenton indicated no relevant financial relationships.
Timothy Wen indicated no relevant financial relationships.
Roxanna Irani indicated no relevant financial relationships.
Uma Mahadevan: AbbVie – Consultant. Boehringer Ingelheim – Consultant. Bristol Myers Squibb – Consultant. Celltrion – Consultant. Eli Lilly – Consultant. Gilead – Consultant. Janssen – Consultant. Pfizer – Consultant. Prometheus Biosciences – Consultant. Protagonist Therapeutics – Consultant. Rani Therpeutics – Consultant. Roivant – Consultant. Takeda – Consultant.
Amy Yu, MD1, Cynthia L. Fenton, MD1, Timothy Wen, MD2, Roxanna A. Irani, MD, PhD2, Uma Mahadevan, MD2, 30, The Effect of Low-Dose Aspirin on Disease Activity in Pregnant Individuals with Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.


